The deadly virus is hitting more and more homes. Here are essentials steps you should take in case it reaches yours.
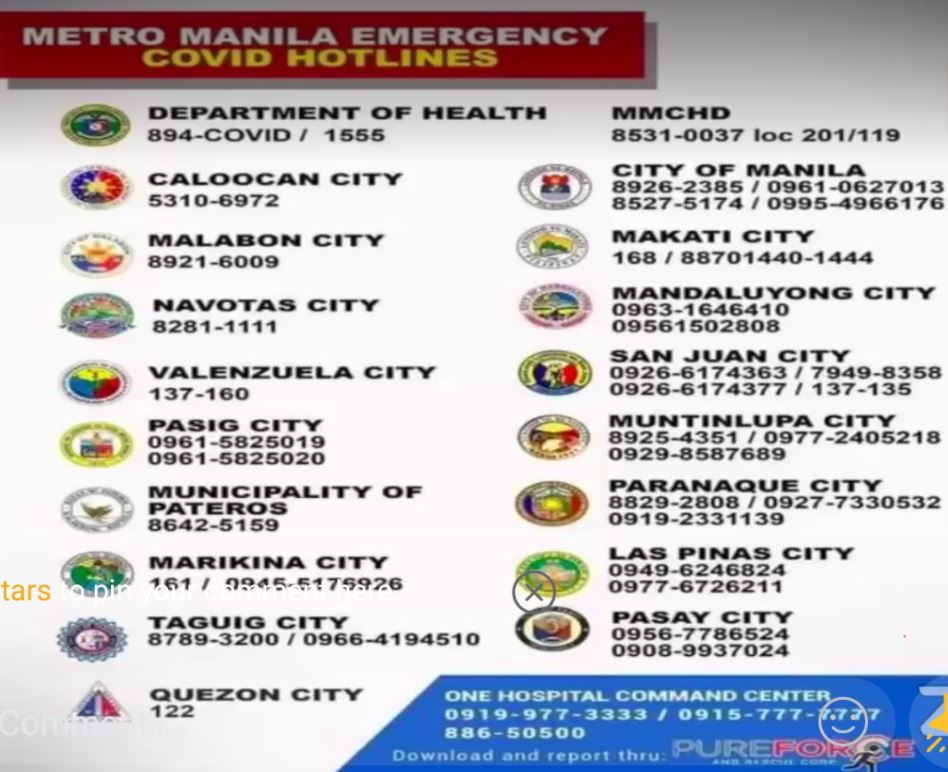
Concern over the alarming surge in COVID-19 cases in the country keeps rising. As of this writing, the Department of Health has reported a total of 904,285 cases with 11,429 new ones logged yesterday. Although the lockdown has been extended in Metro Manila, it is not enough to reduce the number of cases. While there remains no mass testing and vaccine roll-out is starting slow across cities, strictly following safe protocols is our option for now. If someone in your family or in the house gets infected, here the necessary steps to take to care of them according to a recent webinar conducted by the Philippine General Hospital (PGH) Ministry.
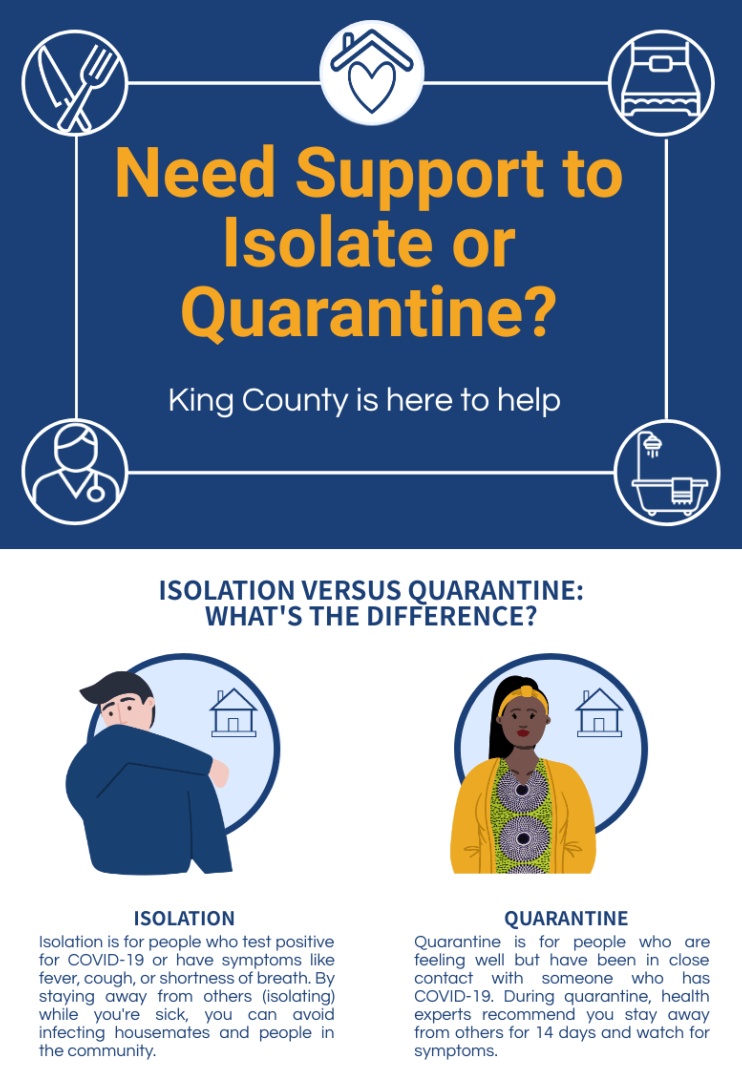
Quarantine or isolation?
Before preparing for home care of a suspected or confirmed COVID-19 patient, know the difference between these two terms first. This will help in identifying the kind of care the patient needs.
Qualifying for quarantine means you have been in contact with people who tested positive for COVID-19. Isolation, on the other hand, means you have been diagnosed with the virus yourself.
Emergency case
Monitor the patient if they are exhibiting any of these signs:
- Persistent pain or pressure in the chest
- Inability to wake or stay awake
- Trouble breathing
- New confusion
- Pale, blue, or graying of lips or nail beds
Seek medical care right away if the patient is showing any of these symptoms.
Qualifications for home care
There are three factors to consider in isolating the confirmed or suspected COVID-19-infected person. One, clinical evaluation of the patient (does the patient qualify for home care); two, evaluation of the home setting (is the home set-up appropriate); and three, the ability to monitor the clinical evolution of a person with COVID-19 at home (can caregivers properly assess the patient).
Qualifications still relies on the degree of the case. This includes risk factors for diseases such as diabetes, obesity, chronic lung disease, and cancer, to name a few.
For asymptomatic or mild cases, hospitalization is not required. They can be monitored at home, given there is no difficulty of breathing, no shortness of breath, and the respiratory rate is less than 30 breaths per minute. Additionally, take note of the patient’s oxygen saturation, which is recorded by an oximeter, as it should reach at least 94 percent.

Preparing for home care
Monitoring the health status of the patient should be done by a public health personnel or trained health worker. If not, the assigned caregiver should remain in contact with a health professional throughout the home care period.
Ideally, only one person should be the caregiver. The latter should be healthy and not at risk of other sicknesses.
The caregiver must prepare a homecare kit. This consists of the following:
- Personal protective equipment (PPEs), medical masks, and single-use or utility gloves
- Cleaning and disinfection liquid for daily use (dilute 45ml of bleach per liter of water)
- A record for vital signs using thermometer, pulse oximeter, and blood pressure (BP) cuff (monitoring must be done every eight hours, or one to three times every day)
- Medications for fever, cough, colds, and patient’s maintenance (for those with comorbidity)
The patient should be isolated in a room and has a separate bathroom than the rest of the house’s dwellers. The room must have good airflow (preferably a window), a small corner for delivery needs like food, and the door must be kept closed at all times.
The rest of the household members should not enter the room of the patient nor physically interact with them.
Ventilate shared spaces like the kitchen and living room, in instances when the patient has to enter these areas. But as much as possible, limit the patient’s movements to their room.

Managing patients
The caregiver must wear a medical mask, protective clothing, and use gloves at all times in caring for the patient and touching the used items.
If utility gloves are used, wash with soap and water and disinfect with 0.1 percent sodium hypochlorite solution. If single-use gloves are used, discard after every use.
The patient should also wear a medical mask. This is changed daily or when wet from secretions. Use tissue when sneezing and or coughing, and must be thrown right away. Never reuse masks and gloves.
The patient should have dedicated eating utensils, linen, and other items for personal use. After every use, wash thoroughly with soap and water.
Contaminated clothes, towels, and linen of the patient must be separately washed. Regular detergent or laundry soap and water will do. Dry these items thoroughly.
Waste from the items of the patient should be discarded separately. Store them in tightly closed bags. It is optional to label them with “contaminated waste” so the trash collectors are aware to handle these with caution. Another option is to bury these wastes, but never burn them.

General care
The caregiver, including the rest of the household, must perform hand hygiene at all times. This should be in line with the World Health Organization’s (WHO) protocols on handwashing. Alcohol is only advised when the hands are not visibly soiled.
Clean and disinfect surfaces and high-touchpoint areas once a day. This includes but is not limited to tables, bed frames, bedroom furniture, doorknobs, bathroom, sink, and toilet areas. Use regular soap and water first. Follow this with a wipe of a disinfectant solution containing 0.1 percent sodium hypochlorite.